Schizophrenia is a chronic and severe mental disorder that affects a person's ability to think, feel, and behave clearly. It is characterized by a range of symptoms that can significantly impair daily functioning, relationships, and overall quality of life. Understanding the diverse manifestations of these symptoms, the complex interplay of factors contributing to its development, and the comprehensive psychiatric care plans essential for management is crucial for providing effective support to individuals living with this condition.
Deciphering the Spectrum of Symptoms
The symptoms of schizophrenia are broadly categorized into positive, negative, and cognitive domains. It's important to recognize that the presentation and severity of these symptoms can vary significantly among individuals and may fluctuate over time.
Positive Symptoms: These are psychotic symptoms that involve an excess or distortion of normal functions. They are often the most noticeable during acute episodes of the illness and can include:
- Delusions: These are fixed, false beliefs that are not based in reality and are not shared by others within the person's culture. Delusions can take various forms, such as persecutory (believing one is being harmed or plotted against), grandiose (believing one has exceptional abilities or importance), referential (believing that common cues or events have special meaning directed at them), or bizarre (beliefs that are clearly implausible).
- Hallucinations: These are sensory experiences that occur without an actual external stimulus. They can involve any of the senses, but auditory hallucinations (hearing voices) are the most common in schizophrenia. These voices may be critical, commanding, or discuss the person's thoughts or actions.
- Disorganized Thinking (Formal Thought Disorder): This manifests in disorganized speech, where the person's thoughts are not logically connected. They may jump from one unrelated topic to another (tangentiality), provide irrelevant answers to questions, speak incoherently ("word salad"), or make up new words (neologisms).
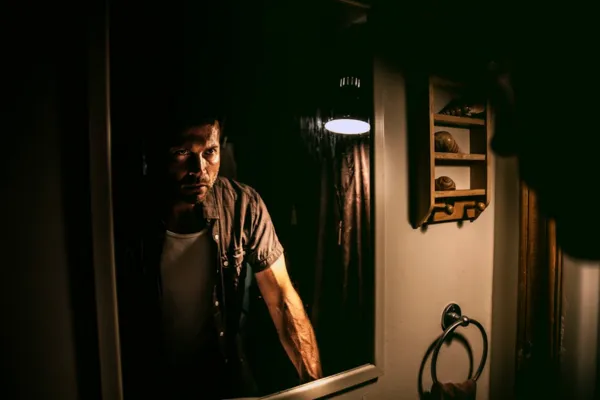
- Disorganized or Abnormal Motor Behavior: This can range from childlike silliness to unpredictable agitation. Catatonic behavior, a more severe form, can involve a decrease in reactivity to the environment, ranging from a rigid posture to complete lack of verbal and motor responses.
Negative Symptoms: These symptoms reflect a reduction or absence of normal functions and can be mistaken for depression or lack of motivation. They tend to be more persistent and can significantly impact daily functioning:
- Flat Affect: Reduced expression of emotions, often characterized by a lack of facial expressions, a monotone voice, and decreased eye contact.
- Alogia: Reduced speech output, characterized by brief and empty replies.
- Avolition: Lack of motivation or ability to initiate and persist in goal-directed activities. This can manifest as poor hygiene, difficulty with work or school, and social withdrawal.
- Anhedonia: Reduced ability to experience pleasure.
- Asociality: Lack of interest in social interactions and withdrawal from social relationships.
Cognitive Symptoms: These involve difficulties with thinking processes and can significantly impact a person's ability to function in daily life. They are often subtle but can be pervasive:
- Impaired Attention: Difficulty focusing and maintaining concentration.
- Memory Deficits: Problems with working memory (holding and manipulating information) and long-term memory.
- Executive Function Deficits: Difficulties with planning, organizing, problem-solving, and abstract thinking.
- Impaired Processing Speed: Slower ability to process information.
Unraveling the Complex Causes
The exact cause of schizophrenia remains unknown, but current research strongly suggests a complex interplay of genetic, neurobiological, and environmental factors:
- Genetic Predisposition: Schizophrenia has a significant genetic component. Individuals with a family history of the disorder have a higher risk of developing it. While no single gene is responsible, multiple genes are believed to contribute to an increased vulnerability.
- Neurobiological and Environmental Factors: Neurobiological factors involve abnormalities in brain structure and function, including differences in brain chemistry (neurotransmitters like dopamine and glutamate), brain circuitry, and brain development. Environmental factors such as complications during pregnancy or birth, exposure to viruses, malnutrition, or significant stress during early development, and certain psychoactive drug use (e.g., cannabis, especially during adolescence) are also thought to increase risk in genetically predisposed individuals.
Neurobiological Factors:
- Neurotransmitter Imbalances: Dysregulation of certain neurotransmitters, particularly dopamine and glutamate, is strongly implicated in the pathophysiology of schizophrenia. The dopamine hypothesis suggests that an excess of dopamine activity in certain brain pathways contributes to positive symptoms. Glutamate, another crucial neurotransmitter, is believed to play a role in both positive and negative symptoms, as well as cognitive deficits.
- Brain Structure and Function Abnormalities: Studies have revealed subtle differences in brain structure and function in individuals with schizophrenia. These may include enlarged ventricles (fluid-filled spaces in the brain), reduced gray matter volume in certain brain regions (such as the prefrontal cortex and temporal lobes), and altered connectivity between different brain areas. These differences are not present in all individuals with schizophrenia and can also be found in some individuals without the disorder, suggesting they contribute to vulnerability rather than being a direct cause.
- Environmental Factors: Various environmental factors during prenatal development, birth, and later life may increase the risk of schizophrenia in genetically predisposed individuals:
- Prenatal and Perinatal Complications: Factors such as maternal malnutrition, viral infections during pregnancy, low birth weight, and birth complications involving oxygen deprivation have been linked to an increased risk.
- Stressful Life Events: While stress is not considered a direct cause, major life stressors, trauma, and social isolation can potentially trigger the onset of psychotic symptoms or exacerbate existing ones in vulnerable individuals.
- Substance Use: The use of certain substances, particularly cannabis and stimulants, has been associated with an increased risk of developing psychosis and schizophrenia, especially in adolescents and young adults with underlying vulnerability.
Constructing Comprehensive Psychiatric Care Plans
Managing schizophrenia effectively requires a long-term, integrated approach that addresses the multifaceted nature of the illness. Psychiatric care plans are individualized and typically involve a combination of the following components:
1. Pharmacological Treatment (Antipsychotic Medications):
Antipsychotic medications are the primary pharmacological treatment for schizophrenia. They work by modulating neurotransmitter activity in the brain, particularly dopamine. These medications can significantly reduce the severity of positive symptoms, such as hallucinations and delusions.
- First-Generation (Typical) Antipsychotics: Older medications that primarily block dopamine receptors. While effective in treating positive symptoms, they are associated with a higher risk of extrapyramidal side effects (EPS), such as muscle stiffness, tremors, and involuntary movements. Examples include haloperidol and chlorpromazine.
- Second-Generation (Atypical) Antipsychotics: Newer medications that affect both dopamine and serotonin receptors. They are generally associated with a lower risk of EPS but have a higher risk of metabolic side effects, such as weight gain, increased blood sugar, and elevated cholesterol. Examples include risperidone, quetiapine, olanzapine, and aripiprazole.
- Long-Acting Injectable Antipsychotics (LAIs): These formulations are administered via injection every few weeks or months, improving medication adherence and reducing the risk of relapse.
Careful monitoring of medication effectiveness and side effects is crucial. Psychiatrists work closely with individuals to find the medication and dosage that provides the best symptom control with the fewest side effects.
2. Psychosocial Therapies:
Psychological and social interventions are essential for addressing negative and cognitive symptoms, improving functioning, and promoting recovery:
- Individual Psychotherapy: Various forms of talk therapy, such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and supportive psychotherapy, can help individuals understand their illness, develop coping strategies for managing symptoms and stress, improve self-esteem, and work towards personal goals. CBT, in particular, can help challenge and modify distorted thinking patterns associated with delusions and hallucinations.
- Social Skills Training: This therapy focuses on improving communication skills, social interaction abilities, and daily living skills, helping individuals reintegrate into the community and build meaningful relationships.
- Family Therapy: Involving family members in the treatment process can provide crucial support, improve communication within the family, reduce expressed emotion (which can trigger relapse), and educate family members about the illness and how to best support their loved one.
- Vocational Rehabilitation and Supported Employment: These programs help individuals with schizophrenia develop job skills, find employment, and maintain their jobs, promoting independence and a sense of purpose.
- Cognitive Remediation: These interventions aim to improve cognitive functions such as attention, memory, and executive skills through structured exercises and strategies.
3. Psychoeducation:
Providing individuals and their families with comprehensive information about schizophrenia, its symptoms, causes, treatment options, and self-management strategies is crucial for promoting understanding, reducing stigma, and fostering active participation in the treatment process.
4. Community Support and Resources:
Access to community-based mental health services, support groups, assertive community treatment teams (for individuals with severe illness and high needs), and housing assistance can provide essential support for daily living, social integration, and relapse prevention.
5. Relapse Prevention Planning:
Developing a proactive plan that identifies early warning signs of relapse, coping strategies to implement, and who to contact in case of worsening symptoms is crucial for minimizing the impact of future episodes and promoting long-term stability.
A Holistic and Collaborative Approach:
Effective management of schizophrenia necessitates a holistic and collaborative approach involving the individual, their family, psychiatrists, therapists, nurses, social workers, and other support professionals. Ongoing assessment, individualized treatment planning, and a focus on recovery and empowerment are essential for helping individuals with schizophrenia lead meaningful and fulfilling lives despite the challenges of this complex disorder.